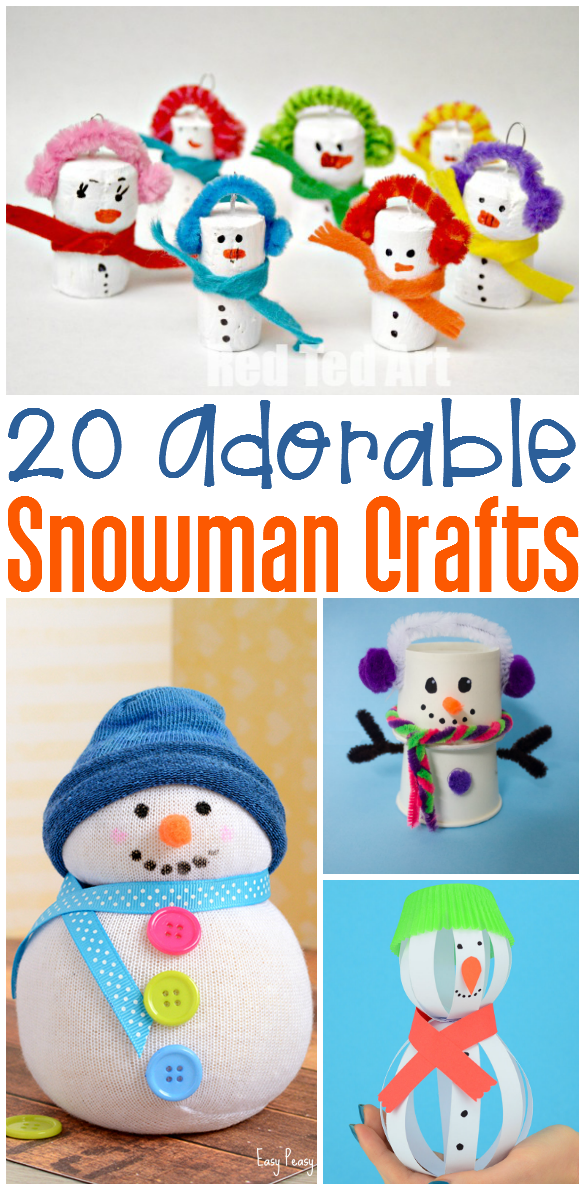
20 Snowman Crafts
Who wants to build a snowman? We do! This week we’ve rounded up some snowman crafts and activities. Each link contains a fun…
Children with disorders of the gastro-intestinal tract commonly experience pain during eating. As a result, the child may develop resistance or anxiety surrounding feeding. The placement of gastric tubes can further complicate the situation as children who require delivery of nutrition via a tube may not have the opportunity to explore the various tastes and textures of food. Typically, when a child does not have an impairment of the GI tract, feeding progresses naturally and is most likely a pleasurable experience. Babies are born with the innate ability to suck and as their gag reflex disappears, the child begins to accept solid foods with variances in texture and taste. Eating becomes social and pleasurable. As the child learns the skills of chewing, including moving food items with the tongue and muscles of the mouth, he develops key skills which will bring about successful eating habits for the future. It is also important to note that the ability to eat helps develop the oral structures necessary for speech production and vice versa. Often times, when children have a negative experience with eating, a bad memory will form. If this is repeated over time, a resistance to try new foods OR anxiety surrounding eating can result. It can be difficult for families to determine exactly when or why a feeding difficulty may have occurred. When a child is not able to eat a diet full of variety in texture and taste, sensory defensiveness may result. This means that the child may exhibit behaviors such as gagging, choking, or avoidance of certain foods based on their perception of the food’s properties.
2) Seek the right professionals.
It is commonly the job of Occupational Therapists (OTs) to help remediate feeding difficulties with children who may or may not have a medical diagnosis. OTs are specifically trained to consider the child’s unique situation as well as the importance of feeding to the family’s daily life. For example, many families with children who have known feeding disorders, may not focus on mealtimes to avoid anxiety and disappointment to the child. There are, however, many ways to work with families on the skills that eating helps to develop in fun and non-threatening ways.
In my book, The Parent’s Guide to OT for Autism and Special Needs, I give an entire chapter of feeding tips. One of the biggest ways to help with feeding consider the meal-time environment. Try to alleviate as much stress from feeding times as possible. Placing pressure on a child to eat or force feeding him may have a negative effect. Keep mealtime conversation light and fun. Encourage your family to listen to calm music or set the table with bright and fun place settings can change the atmosphere into a more positive one.
Let me know what tips you have to help kids with feeding issues.