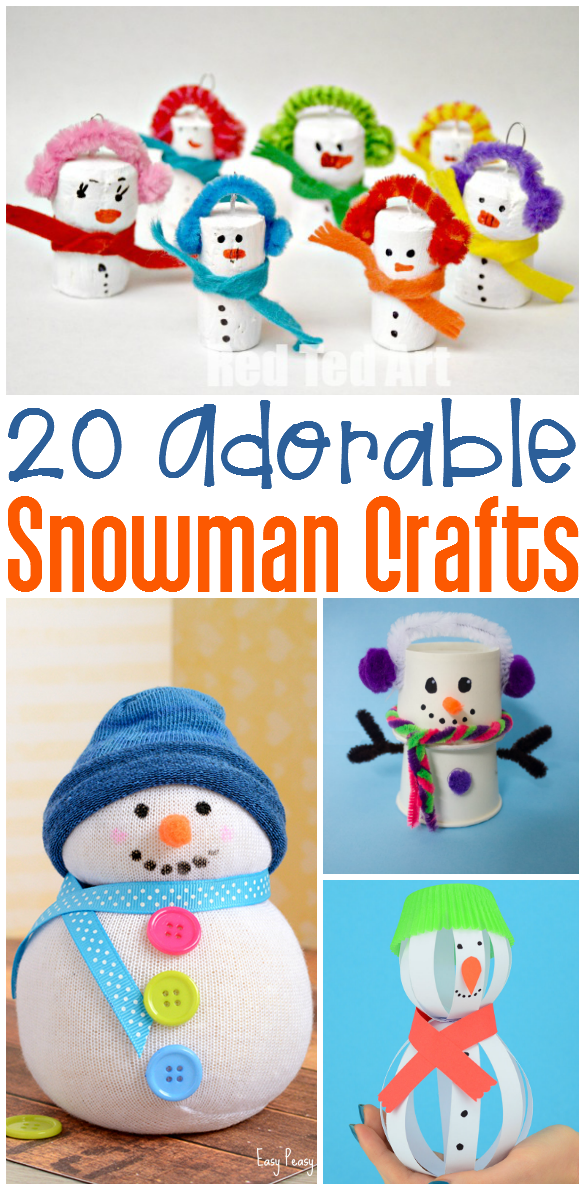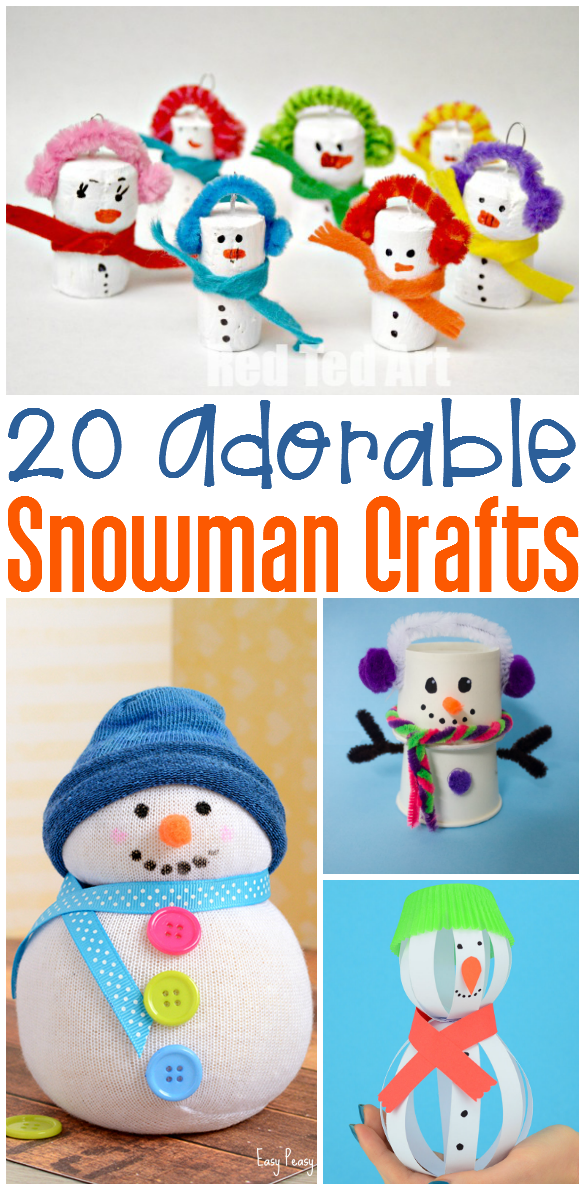
20 Snowman Crafts
Who wants to build a snowman? We do! This week we’ve rounded up some snowman crafts and activities. Each link contains a fun…
Most of us remember the exact place we stood on the morning of the 9/11 attacks. My son was only two and I remember thinking about his future. Thankfully, he was too young to remember but many children faced difficult feelings that they might not have known how to process. The COVID pandemic changed our world forever. Many therapists are reporting a significant increase in behavior-related referrals and sensory processing challenges.
Many of us struggle to make sense of events such as shootings, tragedies, and abuse. Family situations and other everyday circumstances shape us. Feelings of shock, disbelief, sadness, anger, terror, and numbness surface. Everyone deals with traumatic events differently. “I cried all day and could not sleep the night after.” “I had terrible dreams.” “My body feels sick.” How does trauma make you feel? As a parent, teacher, or therapist it’s difficult to know what and how much to discuss with your children. Our kids look to us to help them to feel safe and secure. I struggle with the same issues.
It’s important for us to know the basics of trauma-informed care because using this lens means we need to use whole-system changes and assume EVERY person may have had a traumatic experience that affected them.
Here are some ‘Out of the POCKET’ Tips for dealing with trauma in children.
1 Help children to know that you care and are listening to them. Co-regulation means we share our calm and facilitate warm and caring relationships. Reassure them that you will do what you can to keep them safe. Plan a special activity such as a game, picnic outside, trip to a favorite place, or activity such as fishing. Try to provide solitude and comfort. During your sessions make rules and expectations clear and teach calm-down strategies.
2 Sensory and self-regulation are skills facilitated by OT clinicians. Provide a calm-down area and teach caregivers to do the same at home. Provide a weighted blanket, stuffed animal, or calming sensory input such as music or lavender. If you don’t already have one, this is a wonderful time to make a calming sensory corner or special space for children (and adults) to go when they feel overwhelmed and upset.
To read more in this area, here’s the link to a scientific review of self-regulation interventions relating to toxic stress from birth through adulthood from the US Department of Health and Human Services.
3 Attachment is something that’s an anecdote to trauma. Infants are designed to bond with caregivers. This bond is formed in the early years and impacts the growth, development, and future relationships. Insecure attachments can form with inconsistent, abusive, inappropriate, or neglectful relationships. Look for developmental delays, difficulty coping with stress or anxiety, concentration/attention issues, or social struggles.
4 Remember that children learn through play. Provide pretend play opportunities for children so that they can show sadness and frustration without verbalizing it. To help children to work through emotions, play pretend vet, nurse, or doctor. Many children with a history of trauma struggle to discuss emotions and feelings. Work on building interoception. Here’s a link to my 5 tips to building interoception.

5 Provide outlets for children such as a journal, feelings charts, coloring book, or social stories. Occupational therapists are wonderful educators of self-awareness and regulation training. Here are helpful resources: National Child Traumatic Stress Network; and Infographic from National Association of School Psychologists.
BONUS: Here are some physical manifestations of stress and/or trauma. Remember that behavior IS communication. Always look for a reason for a child’s behavior instead of punishing or taking away calming or play activities.