Me too! I have been doing a ton of research for improving functional outcomes. Some of the same activities over and over get boring for me and for my students. While searching for evidence for my newest course, Building Better Brains Through Movement, I found really cool ideas for our clinic! Yes, I know some of you working in schools have offices (if you’re lucky) that are the size of a closet. Not to worry, find an open area and grab a roll of masking or other colorful tape and let’s go…

Why do we care? Many children who have weak core musculature may need to work in prone and against gravity. Many children with special needs may not complete movements due to physical or sensory difficulties. They may not spend enough time working on crawling or tummy time. Often, they either skipped crawling or moved through the stages quickly. We can identify kids who literally fall out of their chairs when working at their desks. They may lack gross motor coordination for advanced playground movements such as climbing and swinging independently. Other signs include moving the body as a ‘unit’ instead of moving in a segmented way. Ideas to help include working on crawling and obstacle courses in prone. The standing posture results from the sagittal arrangement of the various body segments with respect to gravitational forces. So, the mechanical condition of each vertebral joint is the outcome of the balance between upper body weight and the ligament and muscle’s reactive strength.
Remember in school you learned about the planes of movement? The frontal plane, the sagittal plane, and the transverse plane. We are used to looking for a decreased ability to crossbody midline but we often forget to assess movement in the transverse plane. In my book, Sensorimotor Interventions, I discuss the planes of movement at length. Stand up and place your hands on your hips. Rotate at your waist from right to left. Every time you assess a student, ask them to do the same and take a look at their ability to move the top of their body apart from the bottom (below the waist). 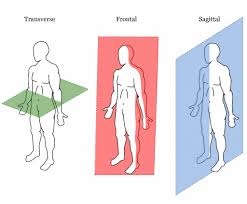
Yes, you read that correctly! Ask the parents to bring in a crunchy snack. Look at the movements of the tongue while chewing. Often, when children struggle with midline crossing, their chewing is more of a ‘munching’ than a rotary chew. Since we treat the ‘whole child,’ we need to understand the impact of decreased ability to move in all planes in all areas. A child’s functional outcomes depend on it! For more information about the development of jaw motion, read the article by Almotiary, et al., (2018). For an article on movement in autism and Developmental Coordination Disorders (DCD) check out the Bhat (2021) article – citation at the bottom of the post.
To be thorough, ask the child to track throughout the visual fields with both eyes. Can the child focus on a moving object? I realize you’re not an optometrist, but you can look at a child’s ability to move their eyes smoothly. If you ever note nystagmus (repetitive, uncontrolled movements), a referral to a physician is ALWAYS needed. Here’s more information on nystagmus from the American Optometric Association. Often children will complain of headaches, fidget, fuss, have watery eyes, or struggle when reading if their eyes are not working properly together. I always encourage parents to see a developmental optometrist when learning disorders are suspected. Here’s more information from the College of Optometrists in Vision Development.
One of my favorite assessment tools is a roll of tape! Look at the student’s ability to walk on the taped line in various ways. Pretend it’s a balance beam and check the ability to walk toe to heel. Ask the student to coordinate the body to jump with both feet to the right and left side of the tape. Invent different ways based on your experience to look at movement patterns in your students. The more you look at the taped line walking, the more patterns you’ll notice in your students. It’s FREE and easy.
Let me know what tips you’ve tried with your students. I love hearing from you!

References
Almotairy, N., Kumar, A., Trulsson, M., & Grigoriadis, A., (2018). Development of the jaw sensorimotor control and chewing – a systematic review. Physiology and Behavior, 194, 456-465.
Bhat, A.N. (2021), Motor Impairment increases in children with autism spectrum disorder as a function of social communication, cognitive and functional impairment, repetitive behavior severity, and comorbid diagnoses: A SPARK Study Report. Autism Research, 14, 202-219.
Talkar, T. et al., (2020). Assessment of speech and fine motor coordination in children with autism spectrum disorder. IEEE Access, 8, 127535-127545.