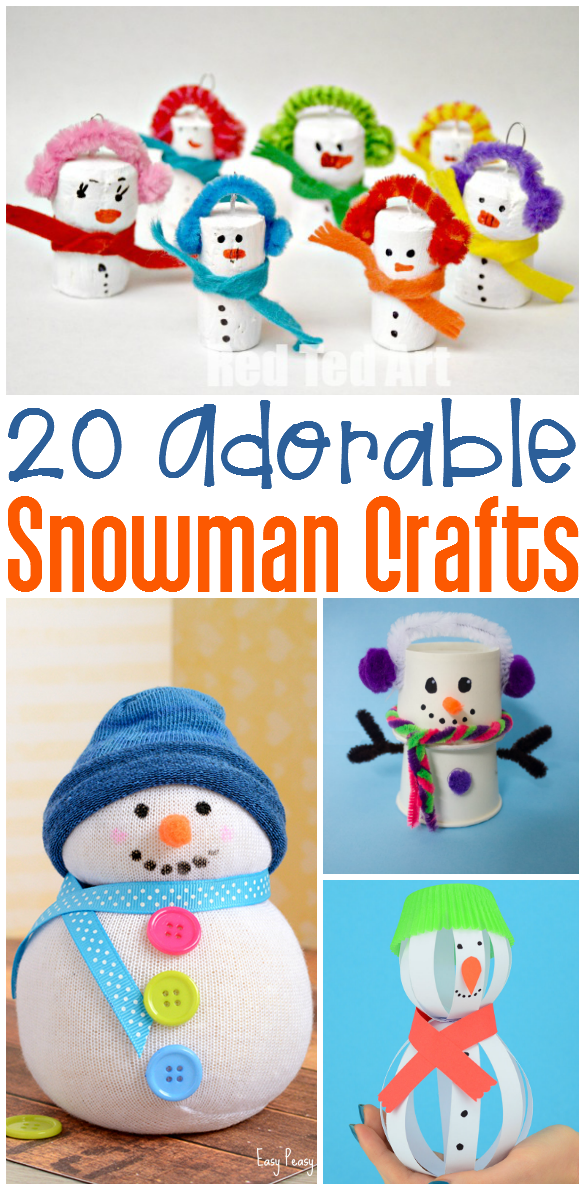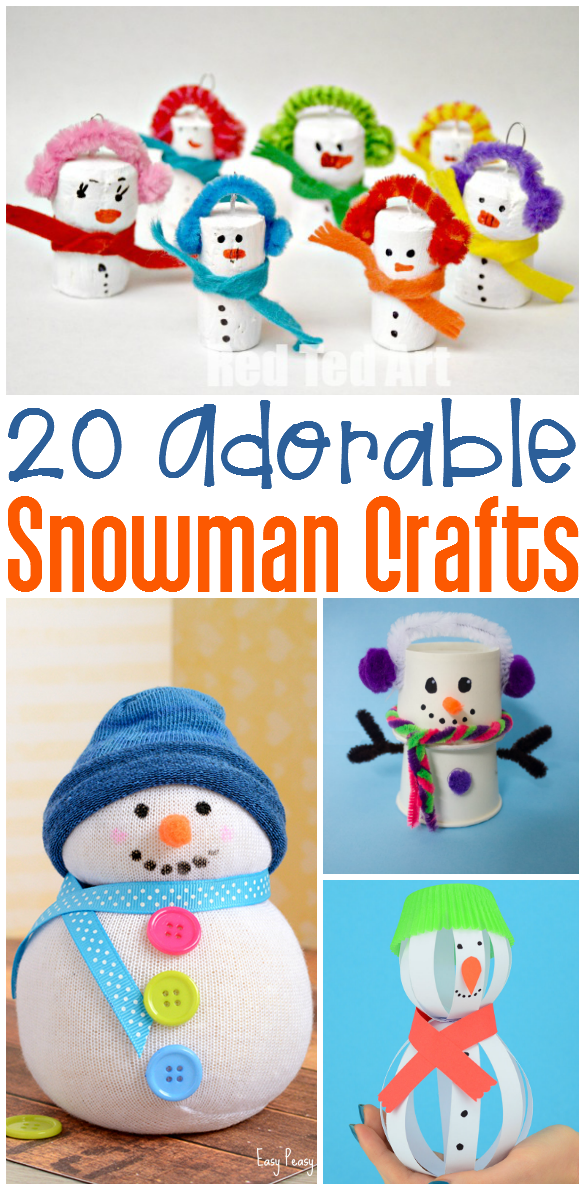
20 Snowman Crafts
Who wants to build a snowman? We do! This week we’ve rounded up some snowman crafts and activities. Each link contains a fun…
In this post, I’ll review the top 5 most asked questions from new OTs who attend my Pediatric OT Primer courses……..
Occupational therapists obtain high levels of training upon graduation. In fact, most OTs graduate with a Master’s degree and some with Doctoral degrees. However, no amount of schooling and fieldwork (the clinical portion of our training) can fully prepare new therapists for the hands-on work of a full caseload. We are skilled at analyzing activities to make them easier or more challenging for our clients and routinely answer questions posed by caregivers. If you’re an OT in the school setting, you also answer queries of teachers and other personnel. In order to provide confident answers, therapists must appear poised and ready.
If you’re looking for new OT graduate tips, here’s the link to our 9 Tips for New OT Graduates post.
1) Do OTs diagnose sensory processing disorders?
The answer is NO. We are not permitted to diagnose any disorder. In fact, the sad truth is that Sensory Processing Disorder is not yet an ‘official’ diagnosis according to the newest DSM (Diagnostic & Statistical Manual). Sensory difficulties are mentioned in the autism category but SPD does not stand alone as a formal diagnosis. OTs can use sensory as a treating diagnosis in an IEP, or on their report but only suggesting it as a reason why treatment goals, modifications, or accommodations are being made. For example, an OT in a clinic setting can evaluate for sensory processing differences and concerns, but the report cannot state, “This OT clinician makes a formal SPD or Sensory Processing Disorder diagnosis.” The OT CAN state the following, “This clinician observed gagging, removal of hand, and facial grimaces when sticky, wet macaroni touched the child’s face and hands indicating sensory avoidance.” Sorry folks, this is a certification rule and licensing issue…..not my doing. If your state or employer tells you differently, I’d suggest contacting your state licensing board, NBCOT, or AOTA.
2) How do I write OT goals?
I know, some of you may be thinking, YES…..this is ME! Guess what, it’s not just you – it’s most of us. We all work with busy and sometimes overwhelming caseloads full of children with different needs and it’s tough to be creative with our goals.
3) When is it OK to work on handwriting?
Handwriting is one of the top reasons for OT referrals — especially in school districts. We are NOT handwriting teachers (although many people think we are) but we are skilled observers. It’s important when receiving a referral for handwriting in clinic and school to determine the reason WHY the child is not performing the skill at age level. We are armed with wonderful assessments that test for other fine and gross motor deficits. Look for patterns and trends. Assess core muscle strength since we know that a strong foundation is required in order for our extremities to function properly. Check out vision. In my newest book “Sensorimotor Interventions” I provide an assessment form with detailed explanations of assessing vision, motor, and core skills. The book contains many interventions with and without suspension equipment. Remember that our vestibular system is intimately intertwined with our visual system.
4) When should I suggest typing/assistive tech accommodations or pencil grippers?
Consider this, children learn to read until third grade and then they read to learn. It’s the same thing with handwriting. As school progresses, the work becomes more difficult. Children are no longer learning to write, their writing is now used for taking notes and completing assignments. When a child KNOWS the information but the handwriting affects his grades, it’s time to consider typing/keyboarding. I’m in NO way suggesting we abandon fine motor skill building, but I do know that a child needs write functionally after third grade.
Pencil grips are another intervention that people have a great deal of confusion around. It’s wonderful to provide an accommodation that assists a child to be more functional, however, we become concerned that kids will become dependent on grippers. I ask you one question, “Do you prefer a certain type/style of writing utensil?” I do…….my writing and hand fatigue becomes a problem when I use a ‘skinny’ pen. I must use a thicker utensil OR one with a larger and softer grip. I encourage therapists to provide a few reasonable gripper styles and let students try them. Look at legibility with and without the grip. By the way, I use FOUR fingers in a ‘death grip’ on my pen, but it works for me 🙂
5) What are the necessities of a sensory corner?
Many therapists have space the size of a small closet from which to work. Some treat in huge gyms with awesome equipment of all sizes and colors. I’ve worked from both over the last 20 years so I understand. When discussing sensory or calm-down areas I suggest the following:
Remember, I offer mentoring sessions and offer many courses online. The newest courses will discuss trauma-informed interventions and confidence boosters/business tips for OTs. Join our mailing list for free activities, news, and discounts.